This week’s case is from a request to see cases of apical periodontitis and chronic apical periodontitis (coming next week). A good definition I found of apical periodontitis is “a spectrum of diseases that occur around the tooth apex, including periapical granuloma, periapical abscess, and periapical (radicular) cyst” (Scheinfeld MH, et al. Teeth: What Radiologists Should Know Radiographics. 2012 Nov;32(7):1927-1944.) Rarefying osteitis is a loss of bone due to inflammation encompassing an abscess, cyst and/or granuloma. Sometimes the word apical or lateral is placed before rarefying osteitis to indicate the location. Apical periodontitis is commonly a clinical diagnosis and rarefying osteitis is commonly a radiographic interpretation. Both entities are the same and are sometimes used interchangeably. The reason both apical periodontitis and rarefying osteitis encompass these three different entities is that (typically) on a radiograph it is not possible to determine the exact nature of the bone loss without a histopathological diagnosis.
Acute apical periodontitis may not be visible radiographically as it takes approximately 8 – 14 days before there is radiographic bone loss. Clinical evidence of severe pain, swelling and/or a sinus tract can lead to a diagnosis of acute apical periodontitis with evident radiographic bone loss.
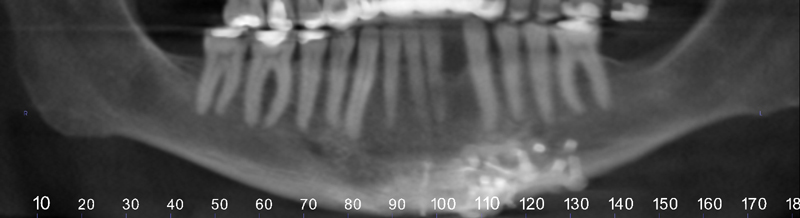
Radiographically, you will see a loss of lamina dura and decreased bone trabeculation (increased radiolucent area) near the source of inflammation. This occurs most commonly at the apex. On the case below, note the loss of lamina dura in the midroot area of the disto-buccal root of the first molar with a radiolucent area of bone superior to here.
 Apical periodontitis or apical rarefying osteitis
Apical periodontitis or apical rarefying osteitis
Disto-buccal root of the first molar.
Next week will be a case of chronic apical periodontitis. If you have any questions, please let me know. Thanks and enjoy!
SPONSOR